Research Highlights
Vol.17, November 2019
A gene-therapy approach for treating spinal cord injury
Delivery of messenger-RNA to the spinal cord through direct injection enhances motor function recovery after spinal cord injury in mice
Damage to a human’s spinal cord — the nervous tissue in the vertebral column — can lead to different levels of paralysis. Spinal cord injury (SCI), usually caused by traffic accidents, sports injuries, falls, or violence, can have a major physical and financial impact on a patient’s live, with lifetime healthcare often required. Keiji Itaka from Tokyo Medical and Dental university and the Kawasaki Institute of Industrial Promotion and colleagues have now investigated an approach for the treatment SCI based on gene therapy, showing promising results in mice.
Recovery from SCI is especially difficult because after the initial loss of nerve cells (neurons), secondary injury effects occur, including inflammation, loss of myelin (the protective layer around nerves) and the formation of an internal scar preventing new neurons to be properly organized. The strategy followed by Itaka and colleagues for treating SCI is to prevent these secondary injuries, so that neural tissues can be kept alive. Specifically, the researchers’ approach is based on the delivery of a therapeutic protein to the spinal cord for neuroprotection and stimulation of neuron activity.
The protein that Itaka and colleagues used is brain-derived neurotropic factor (BNDF), which is known to promote the survival of neurons. Delivery of BNDF to the spinal cord tissue is, however, not straightforward: because the proteins cannot cross the blood–brain barrier, direct injection into the spinal cord instead of intravenous injection is required. In addition, the short half-life and weak tissue penetration of BNDF make it difficult to achieve sufficient therapeutic effects by a single administration of BDNF.
The researchers therefore tried gene therapy for BDNF delivery. Rather than directly injecting BDNF to the spinal cord, delivering the DNA that can produce BDNF is more efficient as it needs to be done only once. Even more efficient is using messenger-RNA (mRNA) instead of DNA; the former has the advantage that it does not need to enter a cell’s nucleus to produce protein,leading to prompt protein production in the cytoplasm.
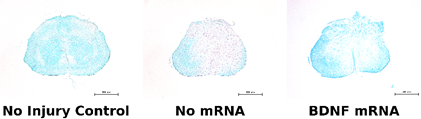
Itaka and colleagues injected BDNF mRNA into the spinal cord of mice that were given SCI by bruising. They monitored the mice’s motor function for a period of 6 weeks after the injury, and observed significant improvement when compared with untreated mice. By the administration of BDNF mRNA, highly-preserved myelinated structures were observed in the injured tissue of spinal cord, representing the neuroprotective effect of BDNF.
The scientists point out that their study is the first to use mRNA therapeutics to the spinal cord, and that for future work, modifications to improve results could include the optimization of the injection protocol and the screening of mRNA encoding different proteins or their combinations. They conclude that “the proof of concept demonstrated … is promising for further research using mRNA to treat SCI.”
Reference:
Crowley, Samuel T. et al. Enhancement of Motor Function Recovery after Spinal Cord Injury in Mice by Delivery of Brain-Derived Neurotrophic Factor mRNA.
Molecular Therapy: Nucleic Acids 17, 465-476 (2019)
https://doi.org/10.1016/j.omtn.2019.06.016
Figure:
[Fig. 1C from the paper]
Figure 1. Delivery of mRNA to the spinal cord in a mouse. Bioluminescent imaging shows the activity of the injected mRNA over time.